Position Statements
About ASTS
From this small group of dedicated individuals, we have grown to represent over 2,000 transplant professionals who are dedicated to saving and improving lives through the transformative power of organ donation and transplant surgery.
Mission Statement
ASTS advances the art and science of transplant surgery through patient care, research, education, and advocacy.
Vision Statement
Saving and improving lives through the transformative power of organ donation and transplant surgery.
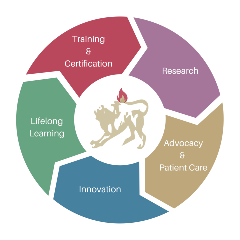
Strategic Plan
We are blazing our own trail for the future under the guidance of our 2022-2027 strategic plan.
Core Values
We operate by these core values:
Integrity - We hold ourselves to a standard of professionalism that includes an awareness of our own imperfections as we seek fairness, justice, and inclusivity. Our behavior is guided by the awareness that we must continuously earn public trust that makes transplantation possible.
Excellence - We commit to setting and achieving ambitious goals as we serve our members, our patients, and society at large.
Forward Focus - We look toward the horizon and support those who are crafting innovative solutions to the problems our members and their patients face.
Respect - We treat our patients, our colleagues, and our collaborators with respect, engaging in constructive debate and supporting each other in our work to save and improve lives.
Diversity - We cultivate the diversity of personal characteristics and individual qualities both in transplantation and among our members. Diversity is integral to the moral code by which we connect lives.
Compassion - We strive to emulate the generosity and courage of the donors and their families who make transplantation possible and to offer hope to our patients.
Join Our Mailing List!
Stay up to date on the latest in transplant surgery.
.png?sfvrsn=2cc04bd3_0)
.png?sfvrsn=93c54bd3_0)
.png?sfvrsn=63cf4bd3_0)
Membership
Join a dedicated group of transplant professionals by becoming a member of ASTS.
Join ASTS.png?sfvrsn=78c04bd3_0)
.png?sfvrsn=586b4bd3_0)
Chimera Chronicles
Hear the stories of transplant legends in their own words.
Explore the chronicles.png?sfvrsn=d0f74dd3_0)
ASTS History: 20th Anniversary
Founding and Early Years
Presidential Reminiscences
Presidential Addresses
The Scientific Program and Scientific Progress
Accreditation of Training Programs, Fellowship Grants and Faculty Development, and Postgraduate Course
The Chimera ASTS Newsletter, Societal Perceptions and Ethical Issues, Politics and Patients
ASTS Membership and Bylaws 1994